CUHK Study Suggests Preoperative Screening for Obstructive Sleep Apnoea to Lower Risk of Postoperative Cardiovascular Events
- admin
- 2019-07-10
- News, Other news
The Faculty of Medicine of The Chinese University of Hong Kong (CUHK) conducted the world’s first study to investigate the association between unrecognised obstructive sleep apnoea (OSA) and postoperative cardiovascular complications. Results showed that patients with unrecognised severe OSA have a two-fold increased risk of postoperative cardiovascular complications compared to those without the disorder. The study has recently been published in the Journal of the American Medical Association (JAMA), suggesting that preoperative OSA screening should be considered in clinical practice to lower the risk of postoperative cardiovascular events.
A study conducted by CUHK Faculty of Medicine shows that patients with unrecognised severe OSA have a two-fold increased risk of postoperative cardiovascular complications compared to those without the disorder. Researchers suggest preoperative OSA screening should be considered in clinical practice to lower the risk of postoperative cardiovascular events.
Anesthetics, sedatives and analgesics exaggerate OSA and pose risks of postoperative cardiovascular complications
OSA is a common form of sleep-disordered breathing. When the patient sleeps, the upper airway is obstructed and leads to a reduction of oxygen in the blood, making it difficult to enter deep sleep and get enough rest. It causes sleep fragmentation, disabling daytime sleepiness and impaired cognitive function. Untreated patients bear a higher risk of cardiovascular diseases, such as heart failure or stroke. According to studies, the prevalence of OSA in middle-aged men is 5% and 2-3% in women.
General anesthetics, sedatives and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilator response to hypoxemia and hypercapnia.
Professor David Shu Cheong HUI, Chairman and Stanley Ho Professor of Respiratory Medicine, Department of Medicine and Therapeutics, Faculty of Medicine at CUHK, remarked, “Each of these events exaggerates OSA and may predispose patients to cardiovascular complications after surgery. Therefore, we need to investigate the association between severe and prolonged nocturnal hypoxemia from OSA and postoperative cardiovascular events, so as to provide evidence and promote better clinical management during the perioperative period.”

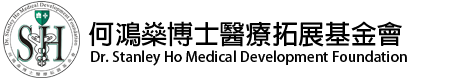
Professor David Shu Cheong HUI (right), Chairman and Stanley Ho Professor of Respiratory Medicine, Department of Medicine and Therapeutics, Faculty of Medicine at CUHK explains Asians tend to have shorter or smaller chin, which is one of the risk factors of OSA.

Professor Matthew Tak Vai CHAN, Professor in the Department of Anaesthesia and Intensive Care, Faculty of Medicine at CUHK says treatment such as oxygen therapy and positive airway pressure may help patients with severe OSA lower the risk of postoperative cardiovascular complications, as conditions like nocturnal hypoxia reduce.
Patients with severe OSA appear with higher risk of postoperative cardiovascular events
The CUHK-led study joined with experts from eight local and overseas hospitals in Malaysia, Singapore, Canada and New Zealand, to investigate the association between OSA and postoperative cardiovascular complications. Two local hospitals involved were Prince of Wales Hospital and Tuen Mun Hospital.
The prospective study recruited and followed 1,218 patients aged 45 or above, without diagnosis of OSA who were undergoing non-cardiac surgery with one or more risk factors of postoperative cardiovascular events. Patients were given preoperative sleep tests and completed a 30-day follow-up after the surgery.
Among the patients, close to 70% (823 patients) had unrecognised OSA and 11% (136 patients) had severe OSA. Within 30 days of surgery, close to 20% of patients appeared with a composite of cardiovascular events including myocardial injury, congestive heart failure, thromboembolism, new atrial fibrillation, stroke, and cardiac death. Below is a breakdown of incidence in different categories of patients.
|
|
Incidence of cardiovascular events |
|---|---|
|
Without OSA (395 patients) |
14% |
|
Severe OSA (136 patients) |
30% |
|
Moderate OSA (235 patients) |
22% |
|
Mild OSA (452 patients) |
19% |
Professor Matthew Tak Vai CHAN, Principal Investigator of the study and Professor in the Department of Anaesthesia and Intensive Care, Faculty of Medicine at CUHK, explained, “Our findings show that the risk of postoperative cardiovascular events in patients with unrecognised severe OSA is significant and twice those without the disorder. Myocardial injury is the most common event among the complications in these patients. It is not uncommon that unrecognised OSA patients are admitted or readmitted to intensive care unit or receive unplanned tracheal intubation or postoperative lung ventilation due to low oxyhemoglobin saturation or nocturnal hypoxia. If these OSA patients were to be recognised before the surgery and provided with appropriate intervention, these happenings might be prevented and ease the burden on patients and hospitals.”
Professor HUI added, “OSA patients often have other health issues such as obesity. Given the evidence displayed in this JAMA study, we believe a preoperative OSA screening should be performed in any non-cardiac surgery. This could be simply done with the STOP-Bang screening tool, a questionnaire which includes assessment of snoring, tiredness, observed apnoea, high blood pressure, body mass index, age, neck circumference, and gender. For those who are found with high-risk, additional monitoring and treatment such as oxygen therapy and positive airway pressure may lower the risk of postoperative cardiovascular complications. These patients should also be transferred for further sleep test and long-term OSA treatment.”
Mr. CHEUNG (left) received sleep test before his knee surgery last year and was diagnosed with severe OSA. He started OSA treatment and the frequencies of snoring and arousals have dropped drastically.
The study was supported by the Health and Medical Research Fund under the Food and Health Bureau of the HKSAR Government.
Source:Faculty of Medicine, The Chinese University of Hong Kong